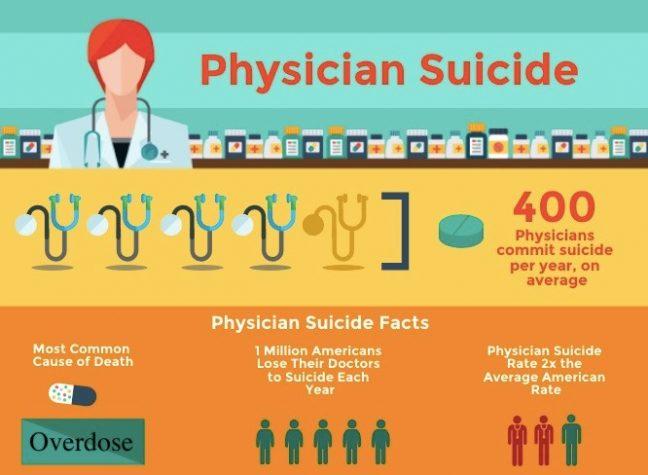
About 400 physicians die by suicide each year, leaving close to one million Americans without their doctors. Around half of physicians that participated in a recent survey reported experiencing burnout, and according to the American Foundation for Suicide Prevention, doctors have a higher rate of suicide risk than the general population.
While factors such as pre-existing mental health conditions and substance abuse can contribute to the problem, emotional exhaustion, fatigue and a lack of self-confidence all stemming from the current culture of medicine are undoubtedly responsible for physician suicide rates. This is especially true for young residents who are now in charge of managing over double the patients they did in medical school. With the current “know-all” culture expected of residents and medical students, reaching out for help becomes difficult and identifying a struggling physician becomes almost impossible.
How is “physician suicide” considered a public health crisis? As stated above, thousands of Americans lose their doctors each year to suicide. With research already showing a shortage of over 100,000 physicians by 2030, the U.S. cannot afford to lose more doctors. Additionally, physician burnout greatly impacts the way doctors practice medicine. Sleep deprivation and the defeating climate in medicine lead to clinical errors, abuse towards patients and a sense of inadequacy within physicians. It puts a strain on the personal relationships physicians have, and it hurts families and friends when suicide does occur.
It’s time for personal conviction vaccination exemptions to go
Medical education programs are not blind to the problem. In 2003, the Accreditation Council for Graduate Medical Education capped work hours to 80 hours per week for all residency training programs which had previously been at 90-120 hours for most specialties. While physician suicide has been largely ignored in the past, medical education programs have begun implementing wellness programs to address the issue.
For example, the Resident Wellness Guide at UW Health includes resources for stress management, emotional wellness, physical fitness, etc. While wellness programs are well-intentioned, their resources are not as likely to be utilized by residents due to a lack of free time and a concern over privacy when seeking mental health counseling. Additionally, they further prove that programs are aware of the tremendous impact the current medical system has on physicians. How can we rely on resilience training and meditation to help doctors cope with medical culture when instead we should be ending the abuse in the medical system which impacts residents and medical students?
The current medical education system needs to shift its management of physician suicide and burnout away from wellness programs and towards radical reform of the abusive nature of medical education and practice. By shining a light on physician suicide, we can hold the medical system responsible.
Anyone can get involved by writing letters to organizations such as the American Medical Association, Association of American Medical Colleges, ACGME and residency education programs. We can question these organizations about how they are changing their atmosphere to relieve stress, burden and limit bullying rather than simply inquiring about resources they have for coping.
As need for mental health services ‘skyrockets,’ university officials look to meet demand
There should be serious repercussions for abusive attending physicians, including termination of employment. The documentary “Do No Harm” by Robyn Symon is the first feature-length film that examines the issue of physician suicide. It could be a required film for all medical education programs to present to their medical students, residents and attending physicians.
For those of us not in the medical field, the simple notion of writing a thank you note to your physician does wonders for their state of mind and sense of purpose. It is pertinent that we help save the lives of those who save lives.
Payge A. Barnard ([email protected]) is an associate research specialist in the psychology department of the University of Wisconsin School of Medicine and Public Health.