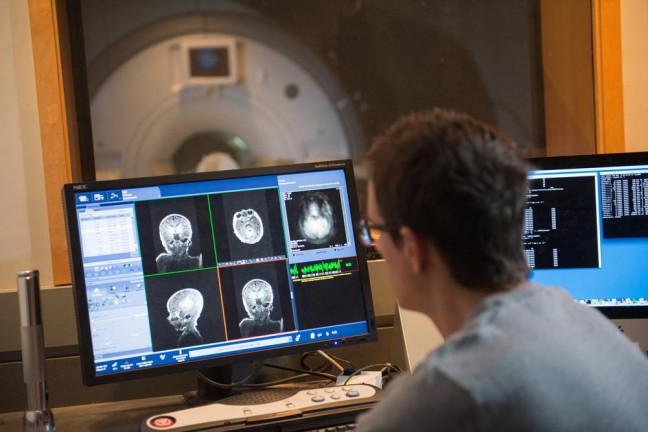
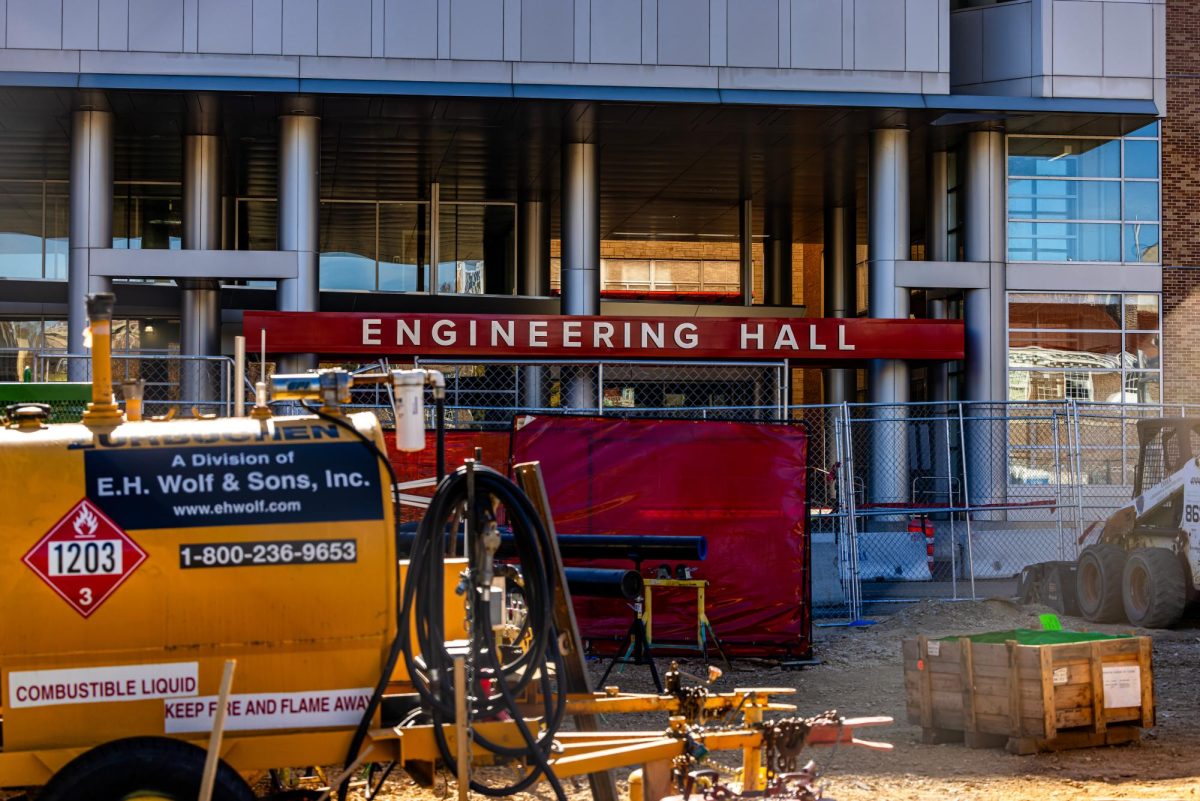
Although it may not be the first condition to come to mind at the mention of chronic conditions, headache-related issues are the primary reasons that patients visit the Department of Neurology at the Medical College of Wisconsin. To expand medical providers’ education about this widespread ailment, UW Health has partnered with the University of Illinois College of Medicine Rockford to create a new fellowship program for headache disorders.
This collaboration may come as a surprise as headaches are not generally known to be life-threatening. But, migraines are shockingly the second leading cause of disability, and yet millions of Americans suffer from headache disorders without adequate treatment.
In fact, the American Headache Society claims that less than a few hours of a physician’s four-year medical education is spent on headache disorders. The organization is concerned that other specialists, like OB-GYN and primary care physicians, end up caring for patients with headaches despite lacking the knowledge to do so as a result of this lack of training.
Racial underrepresentation persists in Madison schools’ honors programs
It is clear that the demand for physicians with headache education vastly exceeds the supply. If patients continue to visit providers without the appropriate knowledge about headache disorders, they will continue to experience frustrations and possible cost inefficiencies.
On the other hand, studies in Korea have shown that patients who visit spine specialists have higher daily costs than those charged by nonspecialists, but their hospital stays and readmission rates are also substantially lower. Specialization in specific ailments may not only lead to improved patient outcomes and clinical efficiency, but it may also decrease the burden of patient volume on other specialties that are not fit to treat headaches.
Drawbacks to expensive medical specializations still exist. For instance, a significant percentage of individuals experience multimorbidity or multiple chronic diseases. While medical specialization may be an extremely efficient method of patient care, excessive specialization may lead to a decline in holistic patient care.
After all, the progression of a chronic illness may be significantly impacted by the presence of another ailment. Different treatments, medications and symptoms may also leave lasting impacts on other disease outcomes. But extensive medical specialization promotes an incomplete approach to patient care.
Considering the economic implications, specialty fellowships offer very limited seats. Even in Madison’s new program, the headache fellowship created by UW Health offers only one seat. Evidently, this will lead to a concentration of specialists in select regions, causing accessibility issues, especially in rural areas. In fact, only 3.1% of neurologists in the U.S. practice in rural areas. As a consequence, the availability of neurologists specialized in headache medicine would be even lower.
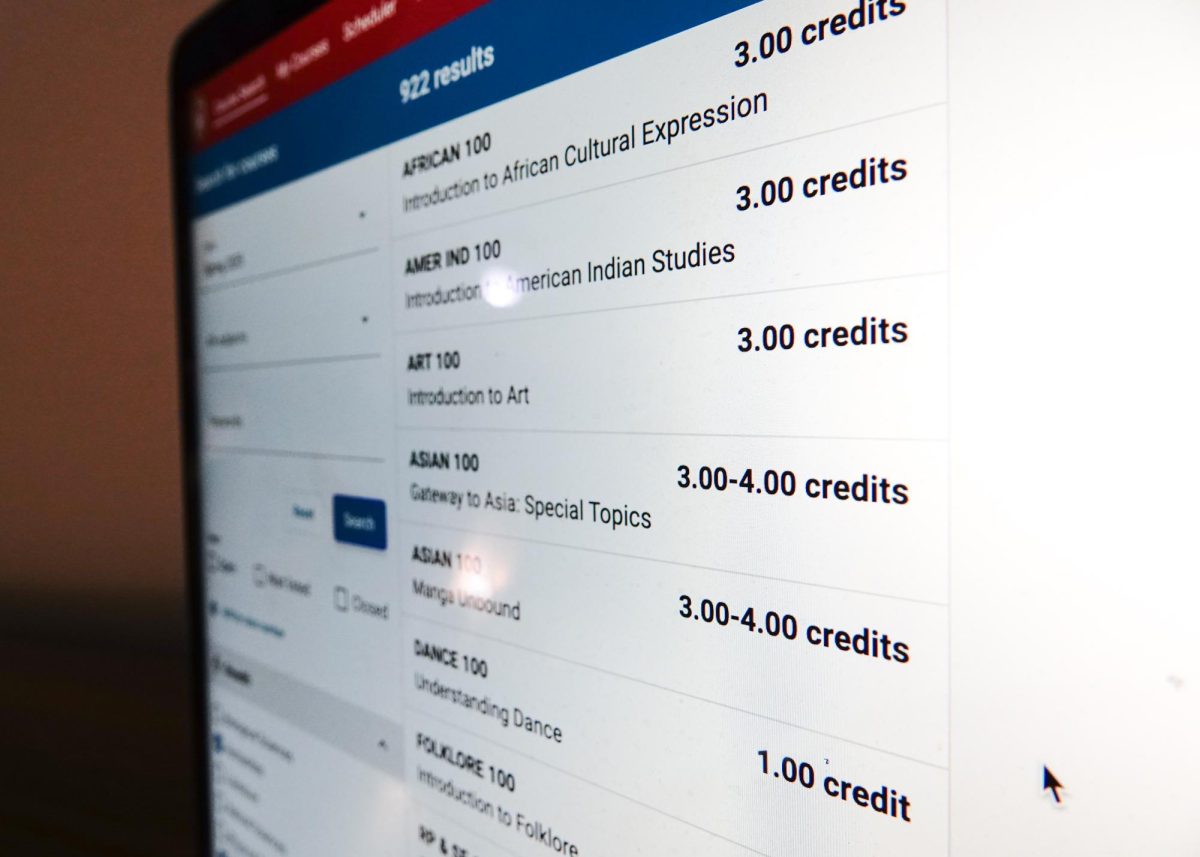
While specializations are important and may benefit patient care efficiency to a certain extent, it is important that we continue to develop tools to improve medical education among all physicians. A possible solution might be increasing the time spent in medical school learning about the most common ailments faced by the American population, including headaches.
Communication between specialists and primary care providers treating the same patient must also be promoted in order to ensure a holistic view of the patient. This calls for research and policy implementations among medical education institutions and healthcare facilities.
Aanikah Parikh ([email protected]) is a freshman studying molecular and cell biology.