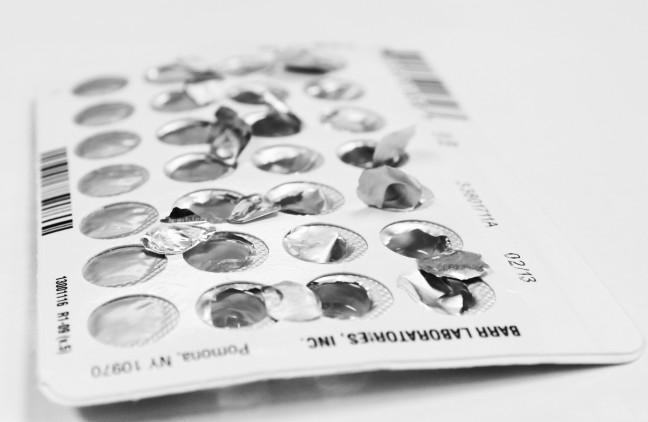
For those participating in heterosexual intimacy, birth control is a huge concern. Particularly for college students, whose priority list probably doesn’t include reproduction, a reliable, equitable and manageable birth control method is essential.
But while female-bodied individuals are presented with a plethora of varied hormonal contraceptives, their male-bodied counterparts have drastically fewer choices.
Hump day: Sexual assault survey fails to fully represent racial, gender identities
Among female contraceptives are the pill, shot, ring, IUD, implant and patch, all which offer reliable birth control and work well in conjunction with non-hormonal methods, such as condoms, cervical caps, withdrawal and fertility awareness method.
But males are limited to vasectomy, condoms and withdrawal. Though vasectomies prove incredibly successful, they are underutilized due to their high cost, surgery requirement and permanent results. Insertive condoms, of course, remain an essential method of birth control and STI prevention, whether alone or used with other methods. Withdrawal, while extremely common and far better than no method at all, remains extremely unreliable — typical use results in a 22 percent failure rate.
Where in the world is birth control for male bodies?
Scientists across the world have taken steps to develop male birth control for decades, but developments in the U.S. have been slow to catch up. Jenny Higgins, a University of Wisconsin gender and women’s studies assistant professor, said pharmaceutical industries and culture are both responsible for slow progress in researching birth control for male bodies.
Very few pharmaceutical companies invest in new contraceptive development because of high costs. Higgins said like medications for heart disease which offer a “best option” only for some people, no single birth control method works for everyone. This makes development cost ineffective and elaborate, especially since hormonal mechanisms involving sperm production can be so complicated, Higgins said.
Hump day: Bisexuality visibility is key to eliminating harmful stigmas
Additionally, underlying cultural assumptions surrounding sex harm progress the U.S. in researching birth control for men. Particularly stifling is the belief that even if birth control were made available to them, men would not use it, Higgins said. She said the stereotype that women are solely responsible for birth control also prevents research.
These cultural norms fail to recognize the importance of both partners’ role in birth control. Only one body can get pregnant, but both bodies involved hold responsibility for prevention of pregnancy. Anyone should have access to contraceptives to feel autonomous control over their sexuality.
The future is now: Vasalgel
Finally in 2010, the nonprofit U.S. Parsemus Foundation purchased a patent for Reversible Inhibition of Sperm Under Guidance invented in India during the 1970s by Sujoy Guha. This low-cost, minimally invasive, reversible procedure shows potential for being an effective temporary male birth control method, according to some studies.
The 15-minute procedure involves injecting a small amount of synthetic gel into the sperm-carrying vas deferens just outside each testicle. After injection, the gel sets in the tube, filtering out the sperm while allowing fluid to pass through. The injection lasts 10 years and can be reversed with a simple injection of baking soda to dissolve the gel, restoring fertility. The Parsemus Foundation call their version of India’s RISUG “Vasalgel” and believe it could be on the market in the U.S. by 2018 or 2020.
Vasalgel, however, does not protect against STIs, and still costs approximately as much as a flat screen TV. Indian clinical trials saw great success with RISUG, but the FDA does not recognize overseas research and the studies must be completed in the U.S. with sufficient sample sizes before approval is possible.
Millions of dollars and careful testing must be accomplished before we have any hope of seeing Vasalgel as a birth control option. In the meantime, use condoms regularly, discuss birth control openly and encourage political leaders to prioritize birth control availability for everyone.