As Americans commemorate those who have risked their lives for their country, three University of Wisconsin psychiatry department faculty have launched a study to further decipher what areas of the brain post traumatic stress disorder affects to produce the most responsive treatment for veterans suffering from the disease.
To understand more fully what happens in the brain during PTSD, Eileen Ahearn, clinical assistant professor in the School of Medicine and Public Health and one of the psychiatrists performing the study, and two UW assistant psychiatry professors, Jack Nitschke and Tracey Smith, will test both soldiers who suffer from PTSD and soldiers who were involved in combat but never developed the disease.
“For those who do have PTSD, we will use both medications and therapy for treatment,” Ahearn said. “MRI testing before and after will hopefully show us which approach works best to stabilize the brain after traumatic events.”
In the wake of the recent incident at Fort Hood in Texas, during which a United States Army psychiatrist shot 13 fellow soldiers, PTSD has gained national attention.
“While it is certainly within the realm of possibility that PTSD somehow prompted the psychiatrist’s actions, more examination of his motives and of his background is necessary,” said Jeremi Suri, professor of history in the College of Letters and Sciences.
Ahearn believes there is much more to the psychiatrist’s story than simply a case of PTSD because hearing about a patient’s trauma is much different and much less distressing than experiencing its detrimental effects firsthand.
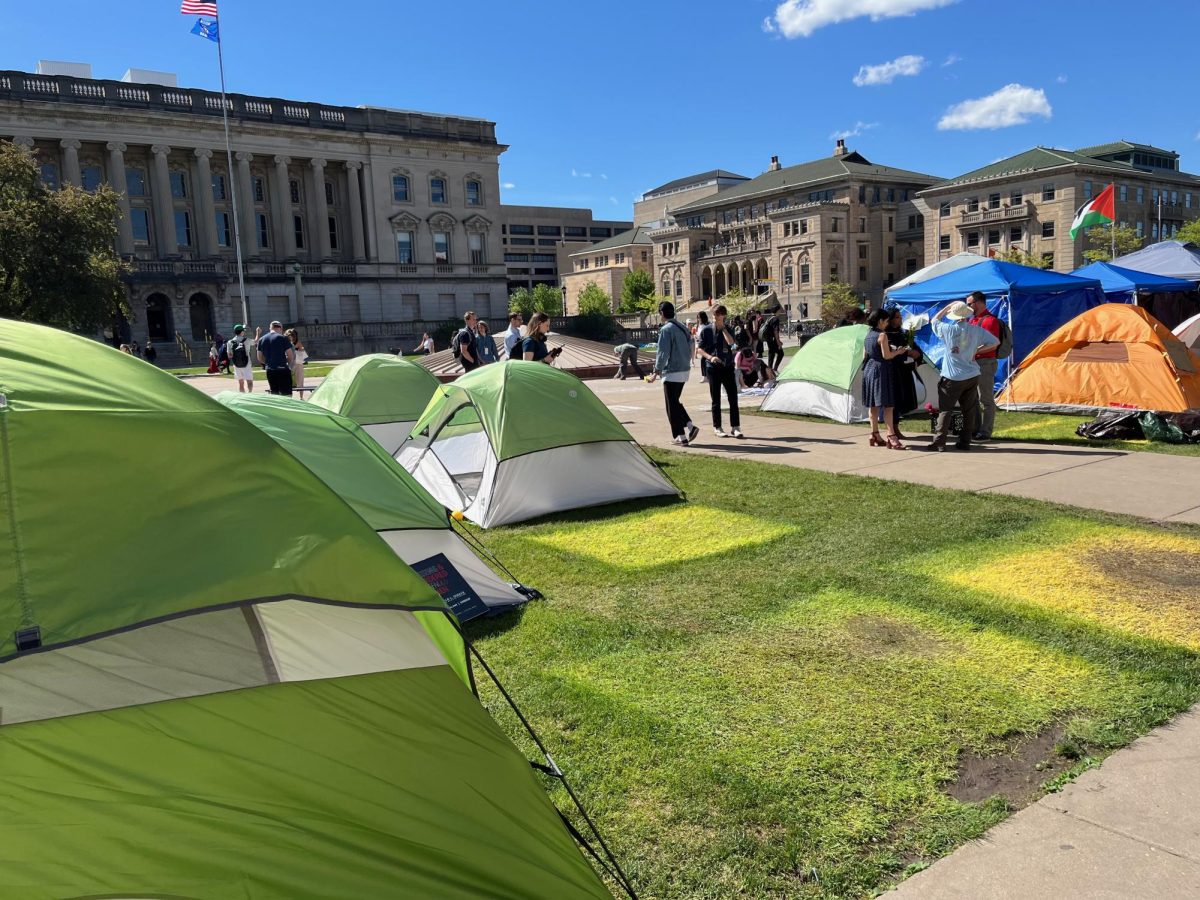
Many veterans dealing with the disease study on campus, so both educators and fellow citizens must consider what these students are going through, Suri said.
Students suffering from PTSD have trouble concentrating and experience detachment from other people, which make it hard to attend class, focus on schoolwork and interact with other students in the class, Ahearn said.
PTSD occurs in some cases when someone is exposed to a life-threatening event, such as seeing a civilian or fellow soldier injured or killed, or they sustain an injury themselves.
Only identified as an actual clinical diagnosis in the past 40 years, PTSD affects 13 to 17 percent of soldiers currently fighting in the wars in Iraq or Afghanistan, or presently attempting to assimilate back into society, Ahearn said.
Common symptoms include intrusive thoughts of traumatic events, nightmares, psychological and physical distress, detachment from relationships and extreme irritability.
While it is hard to predict who will develop PTSD, Ahearn said people with family history of psychiatric disorders, those who have experienced either previous trauma or psychiatric disorders such as depression and anxiety, and females possess a higher risk.
“My hypothesis is that the amount of cases of PTSD is increasing because combat tours are longer,” Suri said. “Constant redeployments result in a life of instability and in an accumulation of symptoms.”
After returning from war, soldiers must integrate back into society and into a less intense and emotional existence, which is a transformation that directly causes PTSD, Suri said. Society offers these soldiers a much different support network and inflicts judgments that were not present within an ordered military life.
UW has partnered with the Madison Veteran’s Hospital to perform a study that aims to develop a clearer picture of what areas abnormally function during PTSD and of how these areas respond to different forms of treatment, Ahearn said.
While University Health Services counseling services do not usually deal with students with PTSD, they do provide support for those returning from war who are struggling with readjustment and attempt to prevent the development of the disease, said Dennis Christoffersen, licensed psychiatrist and clinical director for UHS.
He added since they are not equipped to deal with PTSD, they refer these students to other places in town where they may receive proper treatment, such as the Madison Veteran’s Hospital, the student organization Vets for Vets, or the Madison Vet Center.