As medical experts look to prepare for the winter season, there is uncertainty as to how COVID-19 and influenza will overlap.
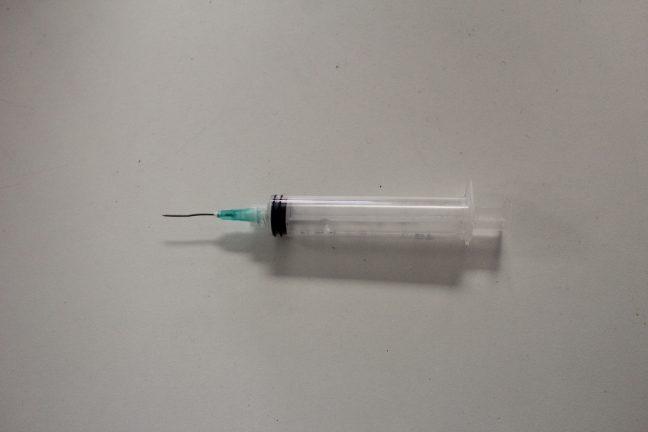
With hospital capacity already limited in states with spiking COVID-19 case counts like Wisconsin according to AP, medical experts are pushing for institutional and personal preparations. The CDC is calling to vaccinate about 65% of American adults and ordered an additional 9.3 million flu shots this year, more than the 500,000 typically purchased for uninsured adults, The New York Times reported.
The ability for hospitals to manage both COVID-19 and flu patients will depend on how strong the flu strain is this year. Professor at UW’s Global Health Institute Dr. Christopher Olsen said though it is nearly impossible to predict how bad a flu season might be, the most recent one in the Southern Hemisphere might give some indication.
“Some people believe that the precautions that have been taken for the sake of COVID in terms of physical distancing, wearing masks, hand washing, limiting in-person events and so on, although aimed at COVID, may in fact have helped with influenza,” Olsen said.
Associate Director for Health Sciences at UW Dr. James Conway said there was talk in spring about setting up a field hospital outdoors, and those plans are being discussed again.
Another difficulty with having two similar respiratory diseases occur at the same time is being able to differentiate between the two. The diseases share mostly the same symptoms, making testing the only clear way to know which disease an individual has.
Olsen said the only true difference between COVID-19 and influenza is the loss of taste and smell with COVID-19. Olsen also warned of the dangers of self-diagnosing these illnesses during an ongoing pandemic.
“People this year shouldn’t be trying to clinically differentiate on their own and then make decisions on their course of actions,” Olsen said. “That’s a dangerous thing to be doing. The message should be if you have COVID or influenza-like illness you should be getting tested.”
The amount of time someone is infectious with COVID-19 is also longer than the flu. While being infectious starts around one to two days prior to clear symptoms for both diseases, it lasts for about 10 days with COVID-19 as opposed to seven with flu.
Medical Director of Infection Control at UW Hospital and Clinics Dr. Nasia Safdar also mentioned how the symptom immediacy of each illness is another way to differentiate between them.
“COVID can occasionally start out as pretty mild symptoms, fairly insidious, whereas with influenza typically people will say ‘I am feeling fine’ and then the next minute they are being hit by a truck,” Safdar said.
Another threat of this combination is contracting both viruses at the same time. A study published in the Journal of the American Medical Association shows nearly 20% of 116 COVID-19 positive patients in the study experienced co-infection with another respiratory virus.
Epidemiologist at the University of California-San Francisco Dr. George Rutherford said in an article having influenza can make a person more susceptible to infection by other pathogens. It is unknown how common co-infection will be, but Conway said it would not be a safe combination for any age group.
“It really stresses us out when any individual gets both those things at the same time,” Conway said. “Even in a completely healthy young person that’s a bad combo.”
American pharmacies like CVS and Walgreens will play a large role in administering the nearly 98 million flu shots estimated to be used this year. CVS is expecting to administer nearly double the number of shots they use in a normal flu season, while Walgreens estimates a 30% to 50% uptick in flu shot demand, according to USA Today.
Medical professionals like UW Preventative Medicine Resident Dr. Devlin Cole emphasized flu shots will both prevent flu outbreaks and lessen the effects of contracting the virus. Cole mentioned how limiting the strength of symptoms will help lower hospital occupancy during the winter season.
“The flu shot is actually really good for vulnerable populations,” Cole said. “We end up seeing less problems with heart disease, less hospitalizations for lung problems and you can keep people with diabetes out of the hospitals.”
Another factor in controlling this potential “twindemic” is having enough staff to manage increases in flu and COVID-19 patients. Wisconsin doctors and nurses had difficulty moving between regional hospitals or units, a problem which Gov. Tony Evers addressed with an emergency order that lessened restrictions on health care worker employment Oct. 1.
The order includes temporary interstate medical license reciprocity, license extensions and allowing for easier renewals. Safdar warned of the effect a pandemic and added flu season will have on healthcare workers.
“The one thing contingency plans don’t always accommodate is what the impact of illness is on the healthcare worker workforce,” Safdar said. “So you can open up beds in other places if you need to but you can’t suddenly find a medical doctor or nurse out of nowhere.”
There is not a clear historical precedent for a scenario where two widespread diseases could simultaneously spread at a rapid pace, with the best example being the 1918 flu pandemic. For Olsen, this lack of recent data is another reason for people to be encouraged to get tested often for COVID-19 and the flu this year.
Olsen said it’s important to look at the epidemiological dynamics of the two diseases this year.
“We’re going to want to have data that we can go back and analyze four to six months from now to be able to better understand how these two viruses played off of one another,” Olsen said.
The medical experts all stressed a need to stay compliant with masking, social distancing and hand washing among other protocols to minimize what will be a taxing winter on hospital resources. Low flu levels in the Southern Hemisphere are largely attributed to these practices.
“We have to remain vigilant and even though we are tired,” Cole said. “We have to recommit to what we know to be working and to be true.”